Penicillin
From Wikipedia, the free encyclopedia
Jump to navigationJump to search
For the Japanese band, see Penicillin (band).
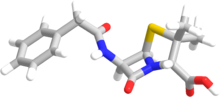
 Penicillin core structure, where "R" is the variable group | |
| Clinical data | |
|---|---|
| AHFS/Drugs.com | Micromedex Detailed Consumer Information |
| Pregnancy category | |
| Routes of administration | Intravenous, intramuscular, by mouth |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Metabolism | liver |
| Elimination half-life | between 0.5 and 56 hours |
| Excretion | Kidneys |
| Identifiers | |
| ChemSpider |
|
| Chemical and physical data | |
| Formula | C9H11N2O4S |
| Molar mass | 243.26 g·mol−1 |
Penicillin (PCN or pen) is a group of antibiotics which include penicillin G (intravenous use), penicillin V (use by mouth), procaine penicillin, and benzathine penicillin (intramuscular use). Penicillin antibiotics were among the first medications to be effective against many bacterial infections caused by staphylococci and streptococci. They are still widely used today, though many types of bacteria have developed resistance following extensive use.
About 10% of people report that they are allergic to penicillin; however, up to 90% of this group may not actually be allergic.[2]Serious allergies only occur in about 0.03%.[2] All penicillins are β-lactam antibiotics.
Penicillin was discovered in 1928 by Scottish scientist Alexander Fleming.[3] People began using it to treat infections in 1942.[4] There are several enhanced penicillin families which are effective against additional bacteria; these include the antistaphylococcal penicillins, aminopenicillins and the antipseudomonal penicillins. They are derived from Penicillium fungi.[5]
Contents
- 1Medical uses
- 2Side effects
- 3Members
- 4Pharmacology
- 5Structure
- 6History
- 7Production
- 8See also
- 9References
- 10Further reading
- 11External links
Medical uses[edit]
The term "penicillin" is often used generically to refer to benzylpenicillin (penicillin G, the original penicillin found in 1928), procaine benzylpenicillin (procaine penicillin), benzathine benzylpenicillin (benzathine penicillin), and phenoxymethylpenicillin (penicillin V). Procaine penicillin and benzathine penicillin have the same antibacterial activity as benzylpenicillin but act for a longer period of time. Phenoxymethylpenicillin is less active against gram-negative bacteria than benzylpenicillin.[6][7] Benzylpenicillin, procaine penicillin and benzathine penicillin can only be given by intravenous or intramuscular injections, but phenoxymethylpenicillin can be given by mouth because of its acidic stability.[8]
Susceptibility[edit]
While the number of penicillin-resistant bacteria is increasing, penicillin can still be used to treat a wide range of infections caused by certain susceptible bacteria, including Streptococci, Staphylococci, Clostridium, Neisseria, and Listeria genera. The following list illustrates minimum inhibitory concentration susceptibility data for a few medically significant bacteria:[9][10]
- Listeria monocytogenes: from less than or equal to 0.06 μg/ml to 0.25 μg/ml
- Neisseria meningitidis: from less than or equal to 0.03 μg/ml to 0.5 μg/ml
- Staphylococcus aureus: from less than or equal to 0.015 μg/ml to more than 32 μg/ml
Side effects[edit]
Main article: Side effects of penicillin
Common (≥ 1% of people) adverse drug reactions associated with use of the penicillins include diarrhoea, hypersensitivity, nausea, rash, neurotoxicity, urticaria, and superinfection (including candidiasis). Infrequent adverse effects (0.1–1% of people) include fever, vomiting, erythema, dermatitis, angioedema, seizures(especially in people with epilepsy), and pseudomembranous colitis.[11] Penicillin can also induce serum sicknessor a serum sickness-like reaction in some individuals. Serum sickness is a type III hypersensitivity reaction that occurs one to three weeks after exposure to drugs including penicillin. It is not a true drug allergy, because allergies are type I hypersensitivity reactions, but repeated exposure to the offending agent can result in an anaphylactic reaction.[medical citation needed] Allergy will occur in 1-10% of people, presenting as a skin rash after exposure. IgE mediated Anaphylaxis will occur in approximately 0.01% of patients.[12][11]
Pain and inflammation at the injection site is also common for parenterally administered benzathine benzylpenicillin, benzylpenicillin, and, to a lesser extent, procaine benzylpenicillin.[medical citation needed]
Members[edit]
| Names | Method of administration | Notes |
|---|---|---|
| Penicillin G, benzylpenicillin | IV or IM | It has high urinary excretion and is produced as a salt of potassium or sodium. |
| Penicillin V, phenoxymethylpenicillin | By mouth | It is less active than benzylpenicillin against Gram-negative bacteria. |
| Benzathine benzylpenicillin, benzathine penicillin G | IM | Benzathine is a stabilizer that causes slower release over two to four weeks. |
| Procaine benzylpenicillin, penicillin G procaine | IM | Slow release. |
Natural penicillins[edit]
- Penicillin G
- Penicillin K
- Penicillin N
- Penicillin O
- Penicillin V
β-lactamase-resistant[edit]
Aminopenicillins[edit]
Carboxypenicillins[edit]
Ureidopenicillins[edit]
β-lactamase inhibitors[edit]
Pharmacology[edit]
Penicillin inhibits activity of enzymes that are needed for the cross linking of peptidoglycans in bacterial cell walls, which is the final step in cell wall biosynthesis. It does this by binding to penicillin binding proteins with the beta-lactam ring, a structure found on penicillin molecules. [13][14]. This causes the cell wall to weaken due to fewer cross links and means water uncontrollably flows into the cell because it cannot maintain the correct osmotic gradient. This results in cell lysis and death.
Some bacteria produce enzymes that breakdown the beta-lactam ring, called beta-lactamases, which make the bacteria resistant to penicillin. Therefore, some penicillin’s are modified or given with other drugs for use against antibiotic resistant bacteria or in immunocompromised patients. Use of clavulanic acid or tazobactam, beta-lactamase inhibitors, alongside penicillin gives penicillin activity against beta-lactamase producing bacteria. Beta lactamase inhibitors irreversibly bind to beta-lactamase preventing it breaking down on beta lactam rings on the antibiotic molecule. Alternatively, flucloxacillin is a modified penicillin that has activity against beta-lactamase producing bacteria due to an acyl side chain that protects the beta lactam ring form beta lactamase. [12]
Mechanism of action[edit]
| This section needs additional citations for verification. Please help improve this article by adding citations to reliable sources. Unsourced material may be challenged and removed. |
Main article: Beta-lactam antibiotic
Bacteria that attempt to grow and divide in the presence of penicillin fail to do so, and instead end up shedding their cell walls.
Penicillin and other β-lactam antibiotics act by inhibiting penicillin-binding proteins, which normally catalyze cross-linking of bacterial cell walls.
Bacteria constantly remodel their peptidoglycan cell walls, simultaneously building and breaking down portions of the cell wall as they grow and divide. β-Lactam antibiotics inhibit the formation of peptidoglycan cross-links in the bacterial cell wall; this is achieved through binding of the four-membered β-lactam ring of penicillin to the enzyme DD-transpeptidase. As a consequence, DD-transpeptidase cannot catalyze formation of these cross-links, and an imbalance between cell wall production and degradation develops, causing the cell to rapidly die.
The enzymes that hydrolyze the peptidoglycan cross-links continue to function, even while those that form such cross-links do not. This weakens the cell wall of the bacterium, and osmotic pressure becomes increasingly uncompensated—eventually causing cell death (cytolysis). In addition, the build-up of peptidoglycan precursors triggers the activation of bacterial cell wall hydrolases and autolysins, which further digest the cell wall's peptidoglycans. The small size of the penicillins increases their potency, by allowing them to penetrate the entire depth of the cell wall. This is in contrast to the glycopeptide antibiotics vancomycin and teicoplanin, which are both much larger than the penicillins.[15]
Gram-positive bacteria are called protoplasts when they lose their cell walls. Gram-negative bacteria do not lose their cell walls completely and are called spheroplasts after treatment with penicillin.
Penicillin shows a synergistic effect with aminoglycosides, since the inhibition of peptidoglycan synthesis allows aminoglycosides to penetrate the bacterial cell wall more easily, allowing their disruption of bacterial protein synthesis within the cell. This results in a lowered MBC for susceptible organisms.[16]
Penicillins, like other β-lactam antibiotics, block not only the division of bacteria, including cyanobacteria, but also the division of cyanelles, the photosynthetic organelles of the glaucophytes, and the division of chloroplasts of bryophytes. In contrast, they have no effect on the plastids of the highly developed vascular plants. This supports the endosymbiotic theory of the evolution of plastid division in land plants.[17]
The chemical structure of penicillin is triggered with a very precise, pH-dependent directed mechanism, effected by a unique spatial assembly of molecular components, which can activate by protonation. It can travel through bodily fluids, targeting and inactivating enzymes responsible for cell-wall synthesis in gram-positive bacteria, meanwhile avoiding the surrounding non-targets. Penicillin can protect itself from spontaneous hydrolysis in the body in its anionic form, while storing its potential as a strong acylating agent, activated only upon approach to the target transpeptidase enzyme and protonated in the active centre. This targeted protonation neutralizes the carboxylic acid moiety, which is weakening of the β-lactam ring N–C(=O) bond, resulting in a self-activation. Specific structural requirements are equated to constructing the perfect mouse trap for catching targeted prey.[18]
Pharmacokinetics[edit]
Penicillin has low protein binding in plasma, the bioavailability of penicillin depends on the type; penicillin G has a low bioavailability, below 30%, whereas penicillin V has a higher bioavailability between 60 and 70%. Penicillin has a short half life and is excreted via the kidneys.[19]
Structure[edit]
Chemical structure of Penicillin G. The sulfur and nitrogen of the five-membered thiazolidine ring are shown in yellow and blue respectively. The image shows that the thiazolidine ring and fused four-membered β-lactam are not in the same plane.
The term "penam" is used to describe the common core skeleton of a member of the penicillins. This core has the molecular formula R-C9H11N2O4S, where R is the variable side chain that differentiates the penicillins from one another. The penam core has a molar mass of 243 g/mol, with larger penicillins having molar mass near 450—for example, cloxacillin has a molar mass of 436 g/mol. The key structural feature of the penicillins is the four-membered β-lactam ring; this structural moiety is essential for penicillin's antibacterial activity. The β-lactam ring is itself fused to a five-membered thiazolidine ring. The fusion of these two rings causes the β-lactam ring to be more reactive than monocyclic β-lactams because the two fused rings distort the β-lactam amide bond and therefore remove the resonance stabilisation normally found in these chemical bonds.[20]
History[edit]
Main article: History of penicillin
Discovery[edit]
Alexander Fleming, who is credited with discovering penicillin in 1928.
Sample of penicillium mould presented by Alexander Fleming to Douglas Macleod, 1935
Starting in the late 19th century there had been many accounts by scientists and physicians on the antibacterial properties of the different types of moulds including the mould penicillium but they were unable to discern what process was causing the effect.[21] The effects of penicillium mould would finally be isolated in 1928 by Scottish scientist Alexander Fleming, in work that seems to have been independent of those earlier observations.[22] Fleming recounted that the date of his discovery of penicillin was on the morning of Friday 28 September 1928.[23] The traditional version of this story describes the discovery as a serendipitousaccident: in his laboratory in the basement of St Mary's Hospital in London (now part of Imperial College), Fleming noticed a Petri dish containing Staphylococci that had been mistakenly left open was contaminated by blue-green mould from an open window, which formed a visible growth.[24] There was a halo of inhibited bacterial growth around the mould. Fleming concluded that the mould released a substance that repressed the growth and caused lysing of the bacteria.[25]
Once Fleming made his discovery he grew a pure culture and discovered it was a Penicillium mould, now known as Penicillium chrysogenum. Fleming coined the term "penicillin" to describe the filtrate of a broth culture of the Penicillium mould. Fleming asked C. J. La Touche to help identify the mould, which he incorrectly identified as Penicillium rubrum(later corrected by Charles Thom). He expressed initial optimism that penicillin would be a useful disinfectant, because of its high potency and minimal toxicity in comparison to antiseptics of the day, and noted its laboratory value in the isolation of Bacillus influenzae (now called Haemophilus influenzae).[24][26]
Fleming was a famously poor communicator and orator, which meant his findings were not initially given much attention.[24] He was unable to convince a chemist to help him extract and stabilize the antibacterial compound found in the broth filtrate. Despite this, he remained interested in the potential use of penicillin and presented a paper entitled "A Medium for the Isolation of Pfeiffer's Bacillus" to the Medical Research Club of London, which was met with little interest and even less enthusiasm by his peers. Had Fleming been more successful at making other scientists interested in his work, penicillin for medicinal use would possibly have been developed years earlier.[24]
Despite the lack of interest of his fellow scientists, he did conduct several experiments on the antibiotic substance he discovered. The most important result proved it was nontoxic in humans by first performing toxicity tests in animals and then on humans. His subsequent experiments on penicillin's response to heat and pH allowed Fleming to increase the stability of the compound.[26] The one test that modern scientists would find missing from his work was the test of penicillin on an infected animal, the results of which would likely have sparked great interest in penicillin and sped its development by almost a decade.[24] The importance of his work has been recognized by the placement of an International Historic Chemical Landmark at the Alexander Fleming Laboratory Museum in London on November 19, 1999.[27]
Medical application[edit]
Florey (pictured), Fleming and Chain shared a Nobel Prize in 1945 for their work on penicillin.
In 1930, Cecil George Paine, a pathologist at the Royal Infirmary in Sheffield, attempted to use penicillin to treat sycosis barbae, eruptions in beard follicles, but was unsuccessful. Moving on to ophthalmia neonatorum, a gonococcal infection in infants, he achieved the first recorded cure with penicillin, on November 25, 1930. He then cured four additional patients (one adult and three infants) of eye infections, and failed to cure a fifth.[28][29][30]
In 1939, Australian scientist Howard Florey (later Baron Florey) and a team of researchers (Ernst Boris Chain, Edward Abraham, Arthur Duncan Gardner, Norman Heatley, Margaret Jennings, J. Orr-Ewing and G. Sanders) at the Sir William Dunn School of Pathology, University of Oxford made progress in showing the in vivo bactericidal action of penicillin.[31][32] In 1940, they showed that penicillin effectively cured bacterial infection in mice.[33][34] In 1941, they treated a policeman, Albert Alexander, with a severe face infection; his condition improved, but then supplies of penicillin ran out and he died. Subsequently, several other patients were treated successfully.[35] In December 1942, survivors of the Cocoanut Grove fire in Boston were the first burn patients to be successfully treated with penicillin.[36]
Mass production[edit]
A technician preparing penicillin in 1943
By late 1940, the Oxford team under Howard Florey had devised a method of mass-producing the drug, but yields remained low.[35] In 1941, Florey and Heatley travelled to the US in order to interest pharmaceutical companies in producing the drug and inform them about their process.[35]
Florey and Chain shared the 1945 Nobel Prize in Medicine with Fleming for their work.
The challenge of mass-producing this drug was daunting. On March 14, 1942, the first patient was treated for streptococcal septicemia with US-made penicillin produced by Merck & Co.[37] Half of the total supply produced at the time was used on that one patient. By June 1942, just enough US penicillin was available to treat ten patients.[38] In July 1943, the War Production Board drew up a plan for the mass distribution of penicillin stocks to Allied troops fighting in Europe.[39] The results of fermentation research on corn steep liquor at the Northern Regional Research Laboratory at Peoria, Illinois, allowed the United States to produce 2.3 million doses in time for the invasion of Normandy in the spring of 1944. After a worldwide search in 1943, a mouldy cantaloupe in a Peoria, Illinois market was found to contain the best strain of mould for production using the corn steep liquor process.[40] Pfizer scientist Jasper H. Kane suggested using a deep-tank fermentation method for producing large quantities of pharmaceutical-grade penicillin.[41][42]Large-scale production resulted from the development of a deep-tank fermentation plant by chemical engineerMargaret Hutchinson Rousseau.[43] As a direct result of the war and the War Production Board, by June 1945, over 646 billion units per year were being produced.[39]
Penicillin was being mass-produced in 1944.
G. Raymond Rettew made a significant contribution to the American war effort by his techniques to produce commercial quantities of penicillin.[44]During World War II, penicillin made a major difference in the number of deaths and amputations caused by infected wounds among Allied forces, saving an estimated 12%–15% of lives.[citation needed] Availability was severely limited, however, by the difficulty of manufacturing large quantities of penicillin and by the rapid renal clearance of the drug, necessitating frequent dosing. Methods for mass production of penicillin were patented by Andrew Jackson Moyer in 1945.[45][46][47] Florey had not patented penicillin, having been advised by Sir Henry Dale that doing so would be unethical.[35]
Penicillin is actively excreted, and about 80% of a penicillin dose is cleared from the body within three to four hours of administration. Indeed, during the early penicillin era, the drug was so scarce and so highly valued that it became common to collect the urine from patients being treated, so that the penicillin in the urine could be isolated and reused.[48] This was not a satisfactory solution, so researchers looked for a way to slow penicillin excretion. They hoped to find a molecule that could compete with penicillin for the organic acid transporter responsible for excretion, such that the transporter would preferentially excrete the competing molecule and the penicillin would be retained. The uricosuric agent probenecid proved to be suitable. When probenecid and penicillin are administered together, probenecid competitively inhibits the excretion of penicillin, increasing penicillin's concentration and prolonging its activity. Eventually, the advent of mass-production techniques and semi-synthetic penicillins resolved the supply issues, so this use of probenecid declined.[48] Probenecid is still useful, however, for certain infections requiring particularly high concentrations of penicillins.[11][needs update]
After World War II, Australia was the first country to make the drug available for civilian use. In the U.S., penicillin was made available to the general public on March 15, 1945.[49]
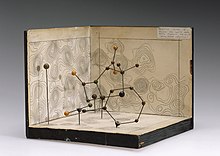
Dorothy Hodgkin determined the chemical structure of penicillin.
Structure determination and total synthesis[edit]
Dorothy Hodgkin's model of penicillin's structure.
The chemical structure of penicillin was first proposed by Edward Abraham in 1942[31] and was later confirmed in 1945 using X-ray crystallography by Dorothy Crowfoot Hodgkin, who was also working at Oxford.[50]She later received the Nobel prize for this and other structure determinations.
Chemist John C. Sheehan at the Massachusetts Institute of Technology(MIT) completed the first chemical synthesis of penicillin in 1957.[51][52][53]Sheehan had started his studies into penicillin synthesis in 1948, and during these investigations developed new methods for the synthesis of peptides, as well as new protecting groups—groups that mask the reactivity of certain functional groups.[53][54] Although the initial synthesis developed by Sheehan was not appropriate for mass production of penicillins, one of the intermediate compounds in Sheehan's synthesis was 6-aminopenicillanic acid (6-APA), the nucleus of penicillin.[53][55][56][page needed]Attaching different groups to the 6-APA 'nucleus' of penicillin allowed the creation of new forms of penicillin.
Developments from penicillin[edit]
The narrow range of treatable diseases or "spectrum of activity" of the penicillins, along with the poor activity of the orally active phenoxymethylpenicillin, led to the search for derivatives of penicillin that could treat a wider range of infections. The isolation of 6-APA, the nucleus of penicillin, allowed for the preparation of semisynthetic penicillins, with various improvements over benzylpenicillin (bioavailability, spectrum, stability, tolerance).
The first major development was ampicillin in 1961. It offered a broader spectrum of activity than either of the original penicillins. Further development yielded β-lactamase-resistant penicillins, including flucloxacillin, dicloxacillin, and methicillin. These were significant for their activity against β-lactamase-producing bacterial species, but were ineffective against the methicillin-resistant Staphylococcus aureus (MRSA) strains that subsequently emerged.[57]
Another development of the line of true penicillins was the antipseudomonal penicillins, such as carbenicillin, ticarcillin, and piperacillin, useful for their activity against Gram-negative bacteria. However, the usefulness of the β-lactam ring was such that related antibiotics, including the mecillinams, the carbapenems and, most important, the cephalosporins, still retain it at the center of their structures.[58]
Production[edit]
A 1957 fermentor (bioreactor) used to grow Penicillium mould.
Penicillin is a secondary metabolite of certain species of Penicillium and is produced when growth of the fungus is inhibited by stress. It is not produced during active growth. Production is also limited by feedback in the synthesis pathway of penicillin.[citation needed]
α-ketoglutarate + AcCoA → homocitrate → L-α-aminoadipic acid→ L-lysine + β-lactam
The by-product, l-lysine, inhibits the production of homocitrate, so the presence of exogenous lysine should be avoided in penicillin production.
The Penicillium cells are grown using a technique called fed-batchculture, in which the cells are constantly subject to stress, which is required for induction of penicillin production. The available carbon sources are also important: glucose inhibits penicillin production, whereas lactose does not. The pH and the levels of nitrogen, lysine, phosphate, and oxygen of the batches must also be carefully controlled.[citation needed]
The biotechnological method of directed evolution has been applied to produce by mutation a large number of Penicillium strains. These techniques include error-prone PCR, DNA shuffling, ITCHY, and strand-overlap PCR.
Semisynthetic penicillins are prepared starting from the penicillin nucleus 6-APA.
Biosynthesis[edit]
Penicillin G biosynthesis
Overall, there are three main and important steps to the biosynthesis of penicillin G (benzylpenicillin).
- The first step is the condensation of three amino acids—L-α-aminoadipic acid, L-cysteine, L-valine into a tripeptide.[59][60][61]Before condensing into the tripeptide, the amino acid L-valine must undergo epimerization to become D-valine.[62][63] The condensed tripeptide is named δ-(L-α-aminoadipyl)-L-cysteine-D-valine (ACV). The condensation reaction and epimerization are both catalyzed by the enzyme δ-(L-α-aminoadipyl)-L-cysteine-D-valine synthetase (ACVS), a nonribosomal peptide synthetase or NRPS.
- The second step in the biosynthesis of penicillin G is the oxidativeconversion of linear ACV into the bicyclic intermediate isopenicillin N by isopenicillin N synthase (IPNS), which is encoded by the gene pcbC.[59][60] Isopenicillin N is a very weak intermediate, because it does not show strong antibiotic activity.[62]
- The final step is a transamidation by isopenicillin N N-acyltransferase, in which the α-aminoadipyl side-chain of isopenicillin N is removed and exchanged for a phenylacetyl side-chain. This reaction is encoded by the gene penDE, which is unique in the process of obtaining penicillins.[59]






























 1306
1306

 被折叠的 条评论
为什么被折叠?
被折叠的 条评论
为什么被折叠?








